Fundamentals
Within Roothea’s expansive living library, the concept of Uterine Fibroids Definition is not merely a clinical description; it stands as a testament to the profound connections between bodily experience, ancestral memory, and the vibrant heritage of textured hair. At its most fundamental, a uterine fibroid, also known as a leiomyoma or myoma, signifies a non-cancerous growth that arises from the muscular wall of the uterus. These growths are quite common, manifesting in various sizes, from a tiny seed to larger than a grapefruit, and can appear as a single entity or in multiples. Their presence can alter the uterus’s shape and size.
The explanation of these growths is straightforward: they are benign tumors composed of smooth muscle cells and connective tissue. While they rarely become cancerous, their existence often brings a spectrum of physical sensations and health considerations. For many, fibroids remain silent, causing no noticeable symptoms. For others, however, the meaning of fibroids translates into tangible discomforts, affecting daily life and overall well-being.
The basic delineation of uterine fibroids typically categorizes them by their location within the uterus:
- Intramural fibroids ❉ These growths reside within the muscular wall of the uterus itself. They represent the most common type and might not present symptoms unless they reach a substantial size.
- Subserosal fibroids ❉ Positioned on the outer surface of the uterus, these fibroids can also extend outward on a stalk, earning them the designation of pedunculated fibroids.
- Submucosal fibroids ❉ Located beneath the uterine lining, these can distort the uterine cavity. Even modest submucosal fibroids can prompt significant bleeding or challenges with conception.
The exact genesis of uterine fibroids remains a subject of ongoing inquiry, yet current understanding points to a complex interplay of genetic and hormonal influences. Estrogen and progesterone, the hormones responsible for thickening the uterine lining during the menstrual cycle, appear to stimulate fibroid growth. This observation finds support in the fact that fibroids commonly emerge during a woman’s reproductive years and frequently diminish after menopause, a period marked by a decline in hormone levels.
Uterine fibroids represent non-cancerous uterine growths, a common occurrence with a diverse range of manifestations and experiences, often influenced by hormonal shifts.
The journey of comprehending uterine fibroids, particularly for those whose lineage is steeped in textured hair traditions, extends beyond mere biological facts. It acknowledges the deep connection between the physical body and the spirit, a connection honored in ancestral care practices. The definition of uterine fibroids, in this light, begins to unveil a larger story of health, resilience, and the enduring wisdom passed down through generations.

Intermediate
Moving beyond the foundational explanation, an intermediate understanding of Uterine Fibroids Definition calls for a deeper look into their prevalence, the spectrum of their impact, and the discernible disparities in experience, particularly within Black and mixed-race communities. The meaning of fibroids expands here to encompass not just their biological characteristics, but their societal and personal ramifications.
A striking aspect of uterine fibroids is their disproportionate incidence among Black women. Research consistently shows that Black women experience fibroids at a significantly higher rate than white women. For instance, studies indicate that approximately 80% of Black women will develop uterine fibroids by age 50, compared to around 70% of white women. This prevalence is not merely a statistical anomaly; it carries substantial implications for health equity and the lived realities of Black women.
Moreover, these growths tend to appear earlier in life for Black women, often by 5.3 years on average, and frequently present with greater size, increased numbers, and more severe symptoms. This earlier onset and heightened severity often translate into a greater likelihood of needing surgical interventions.

Symptoms and Their Expression
While many individuals with fibroids experience no symptoms, for those who do, the manifestations can be debilitating. The significance of these symptoms often dictates the course of care. Common complaints include:
- Heavy or prolonged menstrual bleeding ❉ This can lead to anemia, a condition where the body lacks sufficient healthy red blood cells, resulting in fatigue and weakness.
- Pelvic pain and pressure ❉ Discomfort can range from a dull ache to sharp, intense pain in the lower abdomen or back.
- Frequent urination ❉ Large fibroids can press on the bladder, leading to a constant urge to urinate.
- Constipation or bloating ❉ Pressure on the bowels can interfere with normal digestive function.
- Pain during sexual intercourse ❉ The presence and location of fibroids can cause discomfort during intimate moments.
- Reproductive challenges ❉ Fibroids can sometimes contribute to difficulties with conception, increased rates of miscarriage, or complications during pregnancy and delivery.
The experience of uterine fibroids for Black women often includes earlier onset, greater severity, and a profound impact on daily life, underscoring systemic health disparities.

Factors Influencing Fibroid Development and Experience
The inquiry into why Black women are disproportionately affected by fibroids points to a complex interplay of factors that extend beyond simple genetics. This delineation moves beyond individual biology to consider the broader environment and societal influences.
A growing body of research suggests the role of environmental factors and lifestyle in fibroid development. Studies from the Black Women’s Health Study (BWHS) have explored links between diet, vitamin D insufficiency, and increased fibroid risk. For instance, a higher intake of fruits and vegetables has been associated with a lower risk of fibroids, while a meat-heavy diet may correlate with a heightened risk. Vitamin D deficiency, notably more common in individuals with darker skin tones, has also been connected to increased fibroid risk.
Furthermore, environmental contaminants and chronic stress are emerging as significant considerations. Research indicates that Black communities often face higher exposures to environmental pollutants, and some studies suggest a link between such exposures and fibroid development. The concept of “weathering,” which posits that chronic stress from racial discrimination contributes to the accelerated health deterioration experienced by Black women, is also being examined as a potential contributing factor to fibroid disparities. The relentless pressures of systemic racism and gender discrimination can manifest as physiological stress, impacting overall well-being and potentially influencing health outcomes, including reproductive health.
The intermediate meaning of Uterine Fibroids Definition, then, encompasses not just the biological growth itself, but the broader narrative of health equity, environmental justice, and the enduring effects of societal stressors on the body. It invites a contemplation of how historical circumstances and contemporary realities shape health outcomes within communities of color, especially when considering the holistic well-being that is so deeply intertwined with hair heritage.

Academic
From an academic vantage point, the Uterine Fibroids Definition transcends a mere medical designation, expanding into a complex nexus of biological mechanisms, epidemiological disparities, and deeply rooted socio-cultural contexts. This expert-level explication demands a rigorous examination of the latest research, particularly as it intersects with the lived experiences and ancestral wisdom of Black and mixed-race women. The meaning of uterine fibroids, in this scholarly light, becomes a lens through which to observe broader health inequities and the enduring strength of heritage.
Uterine fibroids, or leiomyomas, are monoclonal tumors arising from the smooth muscle cells of the myometrium, the middle layer of the uterine wall. Their development is intricately linked to steroid hormones, primarily estrogen and progesterone, which act as potent mitogens, driving cellular proliferation and fibroid growth. Fibroids exhibit higher concentrations of estrogen and progesterone receptors than the surrounding healthy myometrium, suggesting an amplified sensitivity to these hormones.
Genetic alterations, particularly in the MED12 gene, are frequently observed in fibroid tissue, pointing to a genetic predisposition that contributes to their pathogenesis. This biological specification underscores a precise understanding of the cellular and molecular underpinnings of these growths.

Epidemiological Disparities and Systemic Contexts
The most compelling and academically significant aspect of uterine fibroids lies in their pronounced racial disparity. Black women face a substantially higher incidence, earlier onset, and increased severity of fibroid disease. By the age of 50, over 80% of Black women will have developed fibroids, a rate significantly higher than that observed in white women. This stark difference is not attributable to biological race, but rather to the cumulative impact of social, structural, and political contexts.
The concept of “weathering,” introduced by Arline T. Geronimus (1992), provides a crucial framework for understanding these disparities. This hypothesis posits that chronic exposure to psychosocial stressors, particularly those stemming from racial discrimination and socioeconomic adversity, leads to premature physiological aging and increased susceptibility to chronic health conditions, including uterine fibroids. The sustained activation of stress response systems can result in allostatic load, a cumulative physiological burden that impacts various bodily systems, potentially influencing hormonal regulation and immune function, which in turn could contribute to fibroid development and growth.
The disproportionate burden of uterine fibroids on Black women is deeply rooted in systemic inequities and the physiological impact of chronic psychosocial stress, particularly racial discrimination.
Consider the pervasive influence of environmental factors. Black communities are disproportionately exposed to environmental toxins, including phthalates and heavy metals, due to residential segregation and proximity to industrial sites. Research indicates that exposure to specific phthalates (MiBP, MBzP, and MEP) was 30% higher in Black women with uterine fibroids compared to white and Hispanic women with the condition, with these differences potentially correlating with fibroid size. (Zota et al.
2014) This case study highlights a critical environmental justice dimension to the Uterine Fibroids Definition, demonstrating how systemic inequities in exposure to pollutants may contribute to health disparities. Such exposures can act as endocrine disruptors, interfering with hormonal balance and cellular processes, thereby potentially influencing fibroid initiation and progression.
Dietary patterns also play a role, with studies suggesting that lower intake of fruits and vegetables, and vitamin D insufficiency, are associated with a higher risk of fibroid formation. Given the socioeconomic determinants of health, access to nutritious food and adequate sunlight exposure (for vitamin D synthesis) can be constrained in marginalized communities, further compounding the risk.

Interconnected Incidences and Broader Implications
The ramifications of uterine fibroids extend beyond physical symptoms, affecting mental health, fertility, and quality of life, particularly for Black women. A national survey revealed that Black women with fibroids were significantly more likely to report interference with physical activities and relationships, and more likely to miss days from work. They also expressed heightened concerns about future fertility and pregnancy following fibroid treatments. This psychosocial impact underscores the need for a holistic approach to care that recognizes the profound connections between physical health, emotional well-being, and ancestral practices of resilience.
The academic definition of uterine fibroids, therefore, cannot be isolated from the broader narrative of Black women’s health. It demands an examination of:
- Medical Bias and Racism ❉ Historically, Black women have faced medical bias and systemic racism, leading to delayed diagnoses, undertreatment, and higher rates of invasive procedures such as hysterectomies. This underscores a critical need for culturally sensitive and equitable healthcare provision.
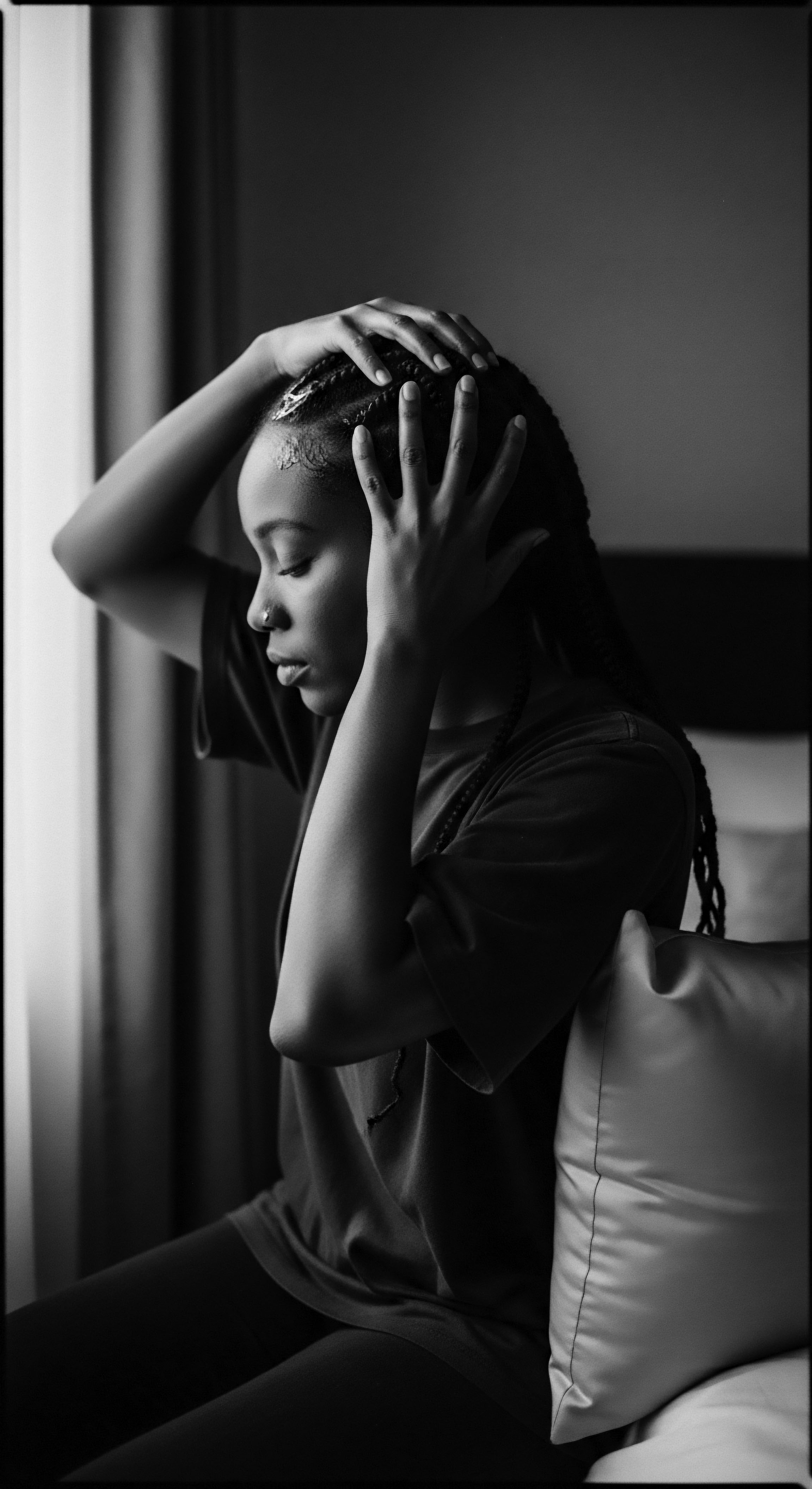
- Mental Health Consequences ❉ The chronic pain, heavy bleeding, and reproductive challenges associated with fibroids can lead to significant psychological distress, including anxiety and depression. The unspoken burden of managing these symptoms while navigating a society that often dismisses Black women’s pain contributes to a silent crisis.
- Reproductive Justice ❉ The disproportionate impact of fibroids on Black women is a matter of reproductive health justice, calling for increased research funding, equitable access to diverse treatment options, and patient-centered care that respects bodily autonomy and addresses systemic barriers.
This comprehensive exploration of Uterine Fibroids Definition from an academic lens not only delineates the biological and epidemiological aspects but also deeply contextualizes them within the historical and ongoing realities of Black women’s health. It calls for a scholarly engagement that acknowledges the interconnectedness of body, environment, and ancestral experience, urging a path toward more just and holistic approaches to well-being.

Reflection on the Heritage of Uterine Fibroids Definition
The journey through the Uterine Fibroids Definition, from its elemental biological description to its complex academic interpretations, finds its most resonant meaning within the Soul of a Strand ethos, particularly through the lens of textured hair heritage. Hair, for Black and mixed-race communities, has always been more than mere adornment; it serves as a living archive, a symbol of identity, resilience, and a deep connection to ancestral wisdom. The experience of uterine fibroids, a condition so profoundly impacting Black women, casts a long shadow that touches upon this very heritage.
When we consider the historical lineage of care, the wisdom of grandmothers and aunties who passed down remedies and self-care rituals, we see echoes of a holistic approach to well-being. These traditions, often rooted in ethnobotanical knowledge and communal support, understood the body as an interconnected system. The burdens of fibroids, manifesting as fatigue, pain, or challenges with fertility, were not just individual ailments; they were concerns shared within the communal fabric, impacting a woman’s ability to engage fully in life, including the cherished rituals of hair care that bind generations.
The stress of navigating health disparities, the quiet pain of being unheard in medical spaces, and the physiological toll of systemic racism, all documented factors in the disproportionate impact of fibroids on Black women, carry a profound weight. This burden can manifest in various ways, sometimes even impacting the vibrancy and health of one’s hair, a visible crown of identity. The meticulous care of textured hair, often a labor of love and a ritual of self-preservation, becomes a quiet act of resistance and a testament to enduring strength in the face of these challenges.
The definition of uterine fibroids, therefore, is not complete without acknowledging the historical and ongoing struggle for health equity that Black women face. It is a call to honor the resilience embedded in every curl and coil, recognizing that the quest for physical well-being is intrinsically linked to the reclamation of ancestral knowledge and the celebration of one’s inherent beauty. The narrative of fibroids, in this context, becomes a powerful reminder of the urgent need for healthcare systems to truly see, hear, and address the unique experiences of Black women, drawing upon both modern science and the profound wisdom of inherited traditions. The threads of health, heritage, and identity are intricately woven, each contributing to the complete, soulful understanding of what it means to be well.

References
- Geronimus, A. T. (1992). The weathering hypothesis and the health of African-American women and infants: Evidence and speculations. Ethnicity & Disease, 2(3), 207-221.
- Stewart, E. A. et al. (2013). The burden of uterine fibroids for African-American women: Results of a national survey. Journal of Women’s Health, 22(12), 996-1002.
- Wise, L. A. et al. (2012). Hair relaxer use and risk of uterine leiomyomata in African American women. American Journal of Epidemiology, 175(5), 432-440.
- Zota, A. R. et al. (2014). Phthalate exposure and uterine leiomyoma in a racially diverse cohort of reproductive-aged women. Environmental Health Perspectives, 122(11), 1188-1194.
- Marsh, E. E. et al. (2018). Burden, prevalence, and treatment of uterine fibroids: A survey of U.S. women. Seminars in Reproductive Medicine, 36(1), 1-10.
- Parker, W. H. (2007). Etiology, symptomatology, and diagnosis of uterine myomas. Fertility and Sterility, 87(4), 725-736.
- Baird, D. D. & Dunson, D. B. (2003). Why is the incidence of uterine leiomyomata so much higher in African Americans? Epidemiology, 14(4), 488-490.
- Eltoukhi, H. M. et al. (2014). The health disparities of uterine fibroids for African American women: A public health issue. American Journal of Obstetrics and Gynecology, 210(3), 205-209.
- Wise, L. A. et al. (2010). Dairy food, calcium, and vitamin D intake and risk of uterine leiomyomata in African American women. American Journal of Epidemiology, 171(4), 432-440.
- Wesselink, A. K. et al. (2021). Ambient air pollution and incidence of uterine leiomyomata in the Black Women’s Health Study. Human Reproduction, 36(6), 1675-1683.