Fundamentals
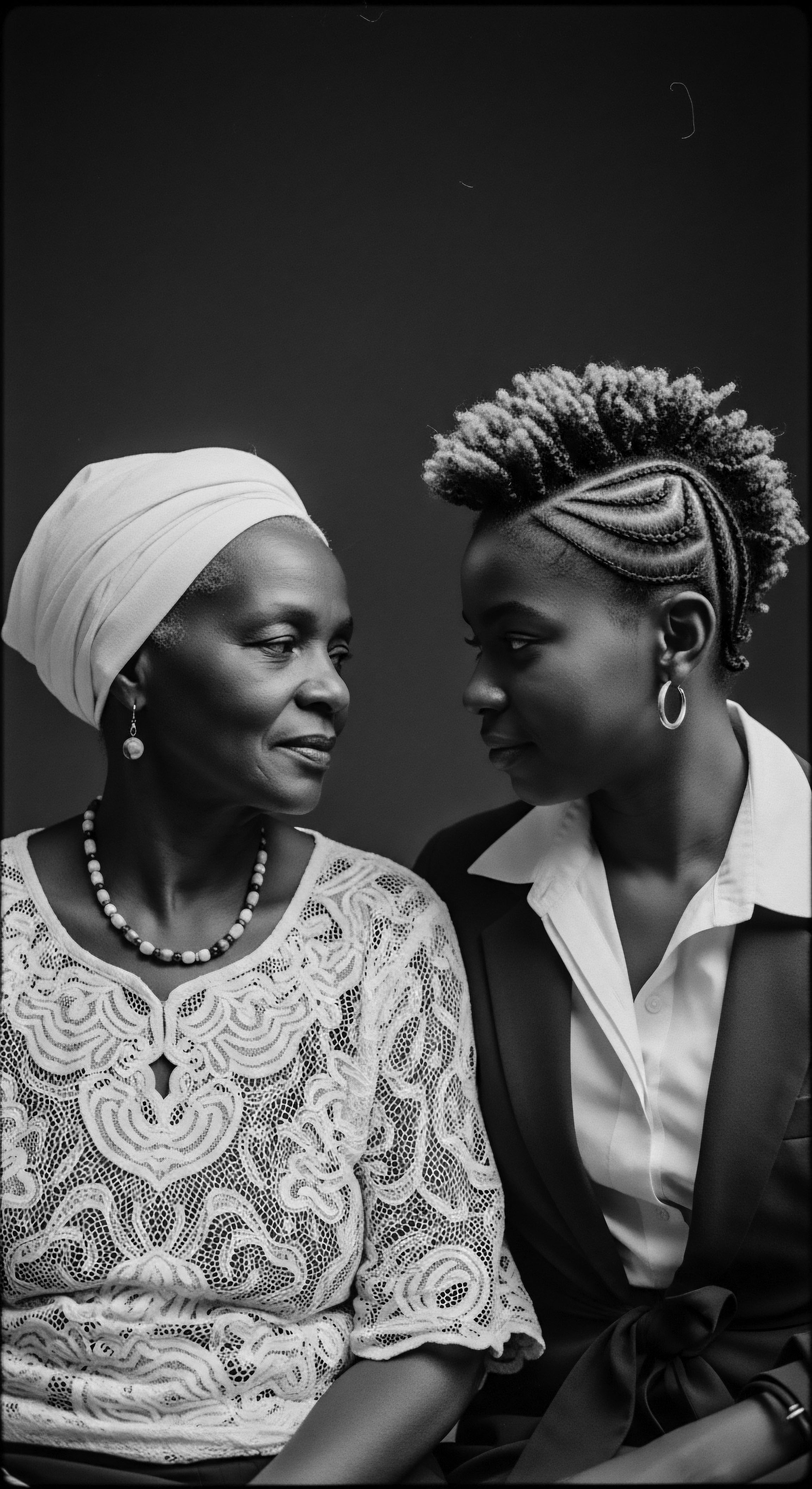
The concept of Fibroid Health Disparities, as we gather it into Roothea’s living library, speaks to the uneven distribution of uterine fibroids and their related burdens across different populations. It is an explanation of how certain groups, particularly Black women, experience these benign growths of the uterus with greater frequency, earlier onset, increased severity of symptoms, and often, more invasive treatment pathways. This delineation is not merely a statement of biological fact; it is a profound observation of how societal structures, historical inequities, and environmental elements intertwine with individual physiology.
At its simplest, this designation points to a clear, observable difference in health outcomes. Uterine fibroids, or leiomyomas, are non-cancerous growths that develop within the muscular wall of the uterus. While they are common, affecting a significant portion of women by age 50, their impact is far from evenly spread.
For Black women, the occurrence is strikingly higher, with a much earlier age of diagnosis and more pronounced symptoms. This reality compels us to look beyond individual choices and toward the broader currents that shape health journeys.

Understanding the Uneven Landscape
To comprehend the meaning of Fibroid Health Disparities, one must acknowledge that health is not merely an individual endeavor, but a reflection of collective histories and prevailing societal conditions. The disproportionate prevalence among Black women, for instance, is not simply a biological anomaly. It points to a complex interplay of factors, many of which are rooted in the legacy of systemic disadvantage.
Fibroid Health Disparities represent a critical imbalance in uterine fibroid prevalence and severity, overwhelmingly affecting Black women due to a confluence of historical, social, and environmental factors.
Consider the numbers that paint a stark picture: nearly a quarter of Black women between 18 and 30 years of age have fibroids, a figure that rises to 60% by age 35. This stands in sharp contrast to the 6% prevalence observed in white women in the younger age bracket. By the age of 50, an estimated 80% of Black women will experience uterine fibroids, compared to approximately 70% of white women. These statistics underscore a profound divergence in health trajectories that demands our thoughtful attention.
- Prevalence ❉ Black women are diagnosed with fibroids approximately three times more often than white women.
- Onset ❉ Fibroids tend to appear at a younger age in Black women, on average 5.3 years earlier.
- Severity ❉ Black women often experience larger, more numerous fibroids and more severe symptoms.
This initial look into Fibroid Health Disparities reveals a deeply embedded pattern. It is a pattern that echoes through generations, influencing not only the physical manifestation of fibroids but also the experiences of care, the paths to diagnosis, and the types of treatments received. The roots of this disparity are complex, extending into the very fabric of social existence.

Intermediate
Moving beyond the foundational comprehension, the intermediate interpretation of Fibroid Health Disparities invites a deeper contemplation of the forces that shape this profound inequity. This is where the interwoven strands of ancestral experience, the enduring spirit of textured hair heritage, and the often-unseen currents of societal influence begin to reveal their collective impact on health outcomes. The term signifies not just a statistical anomaly, but a lived reality, deeply colored by the unique journeys of Black and mixed-race women.

The Echoes of Ancestral Pathways
To understand the meaning of these disparities at an intermediate level, we must acknowledge the historical context that precedes and informs present-day realities. The very notion of health disparities, particularly for Black women, cannot be disconnected from a history of medical exploitation and systemic devaluation. From the painful experiments conducted on enslaved Black women by figures like J.
Marion Sims in the 19th century, often without anesthesia, to the forced sterilizations of women of color in the 20th century, a legacy of mistrust has been sown. This historical backdrop influences how Black women interact with the healthcare system today, contributing to delays in seeking care or a dismissal of symptoms by providers.
The experience of Fibroid Health Disparities for Black women is inextricably linked to historical medical injustices and the enduring legacy of systemic racism within healthcare systems.
The connection to Textured Hair Heritage here is not merely metaphorical; it is a tangible thread in the narrative of Black women’s health. Hair, for many, serves as a profound marker of identity, resilience, and ancestral connection. Yet, certain hair care practices, particularly the historical use of chemical relaxers, have emerged as a subject of scrutiny in relation to fibroid risk.
While no definitive causation has been established, some studies have explored a potential link between the long-term, frequent use of hair relaxers, which contain hormonally-active compounds and harsh chemicals, and an increased risk of fibroids. This suggests that even aspects of cultural expression and beauty practices, when influenced by prevailing societal standards, can become intertwined with health considerations, adding another layer to the complexities of Fibroid Health Disparities.

Intersectional Realities and Environmental Burdens
The interpretation of Fibroid Health Disparities expands to encompass the intersectional realities of race, gender, and socioeconomic status. Black women often face multiple stressors simultaneously, which can contribute to chronic physiological responses. These stressors include:
- Chronic Psychological Stress ❉ Studies indicate higher levels of chronic stress among Black women, stemming from experiences of perceived racism, adverse childhood experiences, and daily societal pressures. This sustained stress can lead to hormonal imbalances, potentially influencing fibroid growth.
- Environmental Exposures ❉ Communities of color are disproportionately exposed to environmental pollutants and toxins due to historical and ongoing environmental racism. Living near industrial facilities, for instance, exposes individuals to higher levels of particulate matter and other harmful chemicals. The impact of these exposures on reproductive health, including fibroid development, is a growing area of concern.
- Socioeconomic Factors ❉ Lower income, limited access to quality healthcare, and disparities in educational attainment are often correlated with higher rates of fibroids and more severe outcomes. These social determinants of health create a landscape where timely diagnosis and access to a full range of treatment options may be hindered.
The significance of these interconnected factors is that they move the conversation beyond a purely biological lens, compelling us to consider the systemic inequities that shape health. The increased rates of hysterectomies and more invasive surgical procedures among Black women, even when accounting for socioeconomic status, further highlight these disparities in treatment. This understanding calls for a holistic approach, one that recognizes the intricate relationship between a woman’s body, her heritage, and the societal currents she navigates.

Academic
The Fibroid Health Disparities represent a complex, deeply embedded public health crisis, manifesting as a significant divergence in the incidence, progression, and management of uterine leiomyomas among ethnoracial groups, with a pronounced and persistent burden on Black women. This delineation extends beyond mere epidemiological observation, requiring an interdisciplinary lens that integrates biological predispositions with the profound influence of social, structural, and historical determinants of health. The explication of this phenomenon necessitates a rigorous examination of the mechanisms through which systemic inequities translate into cellular and physiological alterations, ultimately shaping clinical outcomes.

The Epigenetic Imprint of Lived Experience
The academic meaning of Fibroid Health Disparities posits that the disproportionate burden observed in Black women is not solely attributable to genetic factors, though some studies indicate an ancestral predisposition. Rather, a more comprehensive understanding acknowledges the role of epigenetics ❉ the study of how environmental and behavioral factors can cause changes that affect the way genes work ❉ as a mediating pathway. Chronic exposure to stressors, a hallmark of the Black experience in many societies, can induce epigenetic modifications that influence cellular pathways implicated in fibroid development and growth. This includes the dysregulation of hormonal axes, particularly the hypothalamic-pituitary-adrenal (HPA) axis, leading to altered estrogen and progesterone metabolism, both of which are central to fibroid pathogenesis.
Fibroid Health Disparities for Black women are a profound manifestation of systemic inequities, where chronic psychosocial and environmental stressors converge to influence biological pathways, leading to earlier onset, increased severity, and suboptimal treatment outcomes.
Consider the pervasive impact of perceived racism and discrimination. Research indicates that higher exposure to perceived racism is associated with an increased risk of fibroids among U.S.-born Black women. This form of chronic psychosocial stress is not an abstract concept; it translates into a tangible physiological load, often termed “weathering,” which accelerates the aging process and predisposes individuals to chronic conditions. The physiological response to such stressors involves sustained activation of stress hormones, which in turn can promote inflammation and cellular proliferation within the myometrium, fostering an environment conducive to fibroid growth.

Environmental Racism as a Causal Pathway
A critical, albeit less commonly cited, dimension of this disparity lies in the impact of environmental racism. Black communities are disproportionately located near industrial facilities and hazardous waste sites, leading to elevated exposure to endocrine-disrupting chemicals and air pollutants. These environmental contaminants can mimic or interfere with endogenous hormones, potentially stimulating fibroid growth or altering their cellular behavior.
For instance, a 2018 study by Environmental Protection Agency scientists revealed that people of color faced a 28% higher health burden from particulate pollution, with Black individuals experiencing a 54% greater burden. This constant bombardment of environmental insults contributes to a cumulative risk, eroding overall health and creating vulnerabilities that may exacerbate fibroid development and severity.
The historical context of environmental injustice cannot be overstated. From the legacy of redlining that concentrated Black communities in undesirable, often polluted, urban areas to contemporary policies that permit the siting of polluting industries in these same neighborhoods, a direct lineage exists between discriminatory practices and adverse health outcomes. This systemic exposure, coupled with limited access to fresh, nutrient-dense foods and green spaces ❉ resources often associated with reduced pollution and chronic disease ❉ further compounds the challenge.

The Healthcare System’s Role in Perpetuating Disparities
Beyond the physiological and environmental factors, the academic examination of Fibroid Health Disparities critically analyzes the systemic biases within the healthcare system itself. Black women are more likely to experience delays in diagnosis, receive less comprehensive information about treatment options, and are often steered towards more invasive procedures, such as hysterectomies, at younger ages. Despite the availability of minimally invasive options, Black women are 45% less likely to undergo these procedures compared to white women, even after accounting for other characteristics. This preference for more aggressive interventions carries significant implications for reproductive autonomy and overall quality of life.
The phenomenon of symptom dismissal, where Black patients report their concerns are not taken seriously or their pain is underestimated, contributes to delays in care and a worsening of symptoms by the time a diagnosis is made. This is not merely anecdotal; it is a documented pattern rooted in historical prejudices that falsely claimed Black individuals experienced less pain. Addressing these deeply ingrained biases requires a systemic overhaul, encompassing anti-racism training for healthcare providers, culturally attuned care models, and increased representation of Black clinicians.
The definition of Fibroid Health Disparities, from an academic perspective, therefore, is a call to action. It is a demand for rigorous, culturally sensitive research that explores the multifactorial origins of these inequities, moving beyond simplistic biological explanations to embrace the complex interplay of genetics, environment, and social structures. It is a recognition that true health equity requires dismantling systemic barriers and honoring the historical experiences and ancestral wisdom that shape the health journeys of Black women.

Reflection on the Heritage of Fibroid Health Disparities
As we close this contemplation of Fibroid Health Disparities, the enduring spirit of Roothea’s ‘Soul of a Strand’ ethos reminds us that health, like hair, is deeply intertwined with heritage. The journey of understanding these disparities is not a detached clinical exercise; it is a soulful meditation on resilience, on the echoes of ancestral wisdom, and on the unwavering strength of Black and mixed-race communities. The story of fibroids, particularly its uneven imprint, becomes a profound testament to the enduring impact of history on the living body.
For generations, women of African descent have carried within their bodies not only the biological blueprint of their lineage but also the silent narratives of survival, adaptation, and systemic challenges. The disproportionate prevalence of fibroids among Black women, the earlier onset, and the more severe symptoms are not just medical statistics; they are markers of a journey through time, shaped by environmental stressors, the weight of chronic psychosocial burdens, and often, the historical inadequacies of healthcare systems. This is a story of how the very air breathed, the societal structures navigated, and the historical injustices endured can leave a physical imprint, a testament to the body’s profound connection to its environment and its past.
Yet, within this challenging narrative lies an undeniable strength. The ancestral wisdom, often passed down through oral traditions and communal care practices, holds profound insights into holistic well-being. Before the advent of modern medicine, communities relied on deep connections to the earth and each other, embracing nutrient-dense diets, supportive social networks, and practices that minimized stress. These practices, rooted in a reverence for the body and its natural rhythms, offer a powerful counter-narrative, reminding us that true health is not merely the absence of disease, but a state of harmonious balance, nurtured by connection to one’s heritage and community.
The recognition of Fibroid Health Disparities, therefore, compels us to honor the wisdom of those who came before, to seek healing not just in clinical interventions but in the reclamation of ancestral practices and the dismantling of systemic barriers. It is a call to advocate for equitable care, to ensure that every woman, regardless of her heritage, receives the respect, understanding, and comprehensive treatment she deserves. The legacy of textured hair, in its resilience and beauty, serves as a powerful metaphor for this journey: a testament to enduring strength, an unfolding story of adaptation, and a vibrant declaration of identity that refuses to be diminished. The path forward involves weaving together the threads of scientific understanding with the rich, vibrant fabric of cultural heritage, creating a future where health equity is not just an aspiration, but a lived reality for all.

References
- Marsh, E. E. & Marsh, L. E. (2023). Racial disparities in uterine fibroids and endometriosis: a systematic review and application of social, structural, and political context. Fertility and Sterility, 119(3), 355-363.
- Marsh, E. E. & Marsh, L. E. (2024). Fibroids and Black women’s health: A silent crisis. CanWaCH.
- Marsh, E. E. & Marsh, L. E. (2020). Understanding Racial Disparities for Women with Uterine Fibroids. Michigan Medicine.
- Stewart, E. A. Laughlin-Tommaso, S. K. & Chiaffino, G. (2017). The health disparities of uterine fibroids for African American women: A public health issue. Journal of Women’s Health, 26(10), 1070-1077.
- Marsh, E. E. (2021). Fibroids in Black women: Rates, impact, and more. Medical News Today.
- McLeod Health. (2023). Fibroids: Greater in African-American Women than White. Why? McLeod Health.
- Noel, N. L. et al. (2019). Self-Reported Daily Stress, Squelching of Anger and the Management of Daily Stress and the Prevalence of Uterine Leiomyomata: The Ultrasound Screening Study. Journal of Women’s Health, 28(1), 84-91.
- Ploetzke, M. (2025). Why African American Women Are at Higher Risk for Fibroids. Viva Eve.
- Katon, J. G. Plowden, T. C. & Marsh, E. E. (2023). Racial disparities in uterine fibroids and endometriosis: a systematic review and application of social, structural, and political context. Fertility and Sterility, 119(3), 355-363.
- Stewart, E. A. (2017). Black Women and Uterine Fibroids. Resilient Sisterhood Project.
- Lewis, E. M. (2021). “Mind, Body, & Soul”: The Medical Exploitations Of Black Women In The United States. OpenSIUC.
- Equal Justice Initiative. (2019). Medical Exploitation of Black Women. Equal Justice Initiative.
- Lee, D. (2024). From Property to Power: Confronting the Historic Roots of Black Women’s Health Disparities. Health Affairs Forefront.
- National Academy of Sciences. (2019). Inequity in Consumption of Goods and Services Adds to Racial ❉ Ethnic Disparities in Air Pollution Exposure. Proceedings of the National Academy of Sciences.
- Jardim, N. (2023). Honoring and Preserving Ancestral Wisdom & Healing Traditions. Nicole Jardim.